Covid kills the elderly wherever it finds them
or: why the relatively low mortality rate in Eastern Europe
does not prove any success of the anti-epidemic policies adopted
(second draft: 14.06.2020)
MAIN THESIS
During the first half of May 2020, in France, where the lethal impact of the virus has been massive (and we therefore have a very telling statistical database), the average age of victims at the time of death has been set at 84 years.
At that point, it became clear to me (a Westerner living in post-communist Europe) that there is a strong longevity-mortality connection in the case of the Covid19 pandemic.
If we focus on male longevity (the Covid-19 virus being selective – including sexual selectivity – in its lethal impact), we find that in countries east of the former Iron Curtain, the average life expectancy is below 76 years, while in Western Europe, the average value is clearly over 76.
The virus, obviously, does not “look at your ID”, and is not “interested” in the age of the victims as such, but in the presence of comorbidities (in Hungary, the state administration recently acknowledged that, throughout the official epidemic, only 5% of the registered “Covid-19 deaths” appear to be unrelated to any chronic disease). Well, the incidence of chronic diseases increases exponentially as we move from the so-called “third age” to the “fourth age”, and the present case suggests that – at least in Europe and from the point of view of viral vulnerability – the threshold of the latter could be precisely somewhere around 76 years old.
This is, in my opinion, the main explanatory factor for the surprisingly low mortality rates found in Eastern Europe, where the highest mortality in this study (Moldova: 87 deaths per million) remains lower than that recorded in the least affected Western European state (Austria: 75) – while Greece (17) is obviously both an epidemiological and geopolitical exception.
Though not a trained demographer or statistician myself, in order to make that point, I got acquainted with some statistical methods, and applied them to broad and well-known national data of 21 countries all over Europe[1].
In order to avoid statistical distortion, I chose to include in the study only European countries (21, of which only 5 are outside the EU). They have in common some parameters that ensure that none deviates too radically from the “typical profile” of a European country, namely:
– an official duration of the epidemic as per June 8 between the values of 94 days (Republic of Moldova) and 137 days (France);
– a population between 2.68 million (Republic of Moldova) and 83 million (Germany); and
– a population density between 23 inhabitants/km² (Sweden) and 274 inhabitants/km² (United Kingdom).
I excluded, therefore, countries such as Belgium and the Netherlands (with a population density much above average), but also Norway and Russia (with a population density much below average).
The exclusion of non-European countries is justified by the aim of presenting a politically interpretable study. Globally, of course, the main exceptions to the longevity / mortality correlation we have discovered are in East Asia. But in those societies, the mere decades of their coexistence with corona viruses, as well as the average level of technological and cultural readiness for viral threats, in my opinion, makes it difficult to compare their results with the results achieved by European societies which even in the most favourable case (among major countries, probably Germany), have showed their structural limits during this crisis.
That is why, when we question the effectiveness of anti-epidemic policies adopted in different European countries, “cross-cutting” comparisons (combining East and West figures) should be rejected from the outset[2]. It makes no sense, for example, to compare the mortality recorded in Sweden (with a male life expectancy close to 81) and in Romania (where it is below 73). Sweden is worth comparing to France, Italy, Spain or Denmark (and only in the last comparison does it come out significantly worse – which could be related to the fact that, for reasons still unclear, Denmark has a male longevity three years lower). And the results in Romania (the country with the harshest quarantine in Europe) are worth comparing with those in Hungary (a country that applied a more moderate quarantine) or Belarus (which did not apply any quarantine).
From all the above legitimate comparisons, it appears that quarantine policies do not have much epidemiological impact – as world-renowned virologists such as Prof. D. Raoult of France or S. Bhakdi of Germany had already predicted at the very beginning of the crisis[3].
The logic of this study has already been virulently attacked on social media by propagandists from various Eastern European governments. Those governments, after unnecessarily monkeying the delusional policies observed in the West (except Sweden), are trying to present the balance sheet of each Eastern European country as a great managerial success. Which, personally, would not bother me (since I am not a citizen of those states), if it did not involve the defence of an inefficient, socio-economically devastating and freedom-killing model of “crisis management”.

COUNTER-ARGUMENTS
Among the counter-arguments often brought by the aforementioned propagandists, we find recurring elements taken from “popular wisdom”, which, in general, can be grouped into two main categories:
- The states with better results (or results disturbing for the defended model) lied, i.e. manipulated the numbers.
- If in some countries better results have been obtained despite lighter quarantines or without quarantines, it is related to the “level of discipline” of the population of those countries.
We could talk extensively about the reliability of the sources used in the present study, but we can also summarize: both sets of arguments hit the same statistical wall, that is, i.e. the fact that we can always suspect a country of dishonesty or lack of discipline, but we go into delirium the moment we begin to generalize that suspicion to entire series of states, seemingly chosen at random (but, in fact, according to our argumentative interests: what epistemologists call confirmation bias). In reality, it is clear that there is no conspiracy between Sweden, Switzerland, Iceland, the Netherlands and Belarus to camouflage deaths in countries with little or no quarantine. And, even if the cliché of the “undisciplined Romanian” is widely accepted, the suspicion that Hungarians would be more or less disciplined than the citizens of Belarus seems counter-intuitive.
Another popular explanation must be categorically rejected. In various post-communist countries, those nostalgic for pre-1990 regimes (strangely reinforced by various late anti-communists who could not resist the temptation to find motives of national pride even in their country’s communist past) evoked the role of communist compulsory vaccination policies (often continued by the post-1990 regimes) in building up the “average immunity” of Eastern populations. Their argument was ab ovo destroyed by Prof. Raoult, who, in an April 14 interview, noted that such a “surprisingly” low level of relative mortality compared to the averages found in the West was characteristic, not only for Eastern Europe (which he does not deal with much), but for the vast majority of poor countries. Therefore, another study would be needed to compare the vaccination policies of the last 80 years in those countries – but it is very unlikely to find, outside the post-Soviet and communist world, the same substances and / or frequencies of administration, at least such substances and / or frequencies which are also radically different from those observed in Western populations with high Covid-19 mortality. The real common denominator of the countries “exempt” from high Covid-19 mortality is, thus, poverty – and its demographic consequences: low longevity (as confirmed by the present study), but maybe also overconsumption of new and unreliable expensive medicine.
At this precise point, we run into another widespread prejudice, which we have encountered in interlocutors from Hungary, Romania and Russia: the elderly in the West (“because” they live longer) would be healthier. Here, any response in re would require additional large scale studies. But we can already intuitively object that, in fact, we are dealing in the West with a phenomenon of concealment of old age and death – concealment for which there are also recently imported cultural preconditions in Eastern Europe, but without the necessary financial means to implement it. In other terms: the old westerners we see are the healthy ones, very visible, because their high income level also opens them the gates of mass tourism, including abroad). But the same old Westerners, after losing their biological autonomy, disappear – not by being taken to the cemetery, as is often the case in post-communist countries, but to nursing homes, where they can be kept for years in de facto intermediate states between life and death. This is precisely the demographic category that, regardless of location, provided the bulk of the Covid-19 “specific” mortality victims. And given the (now already well-known) role of nursing homes in the propagation of the virus, large recourse to nursing homes might actually be one of those richness-conditioned bad habits (parallel to medicinal overconsumption) which made the West’s disadvantage even worse.

METHODOLOGICAL REMARKS
Comparing national figures and national averages has many downsides. One of them (cf. supra) is the risk of statistical distortion due to the heterogeneity of nation-states (in terms of total population, density etc.). I have tried to avoid such distortions by excluding demographically atypical countries.
Another one is that it leads to disregarding state-internal regional/local differences, which, in the case of the health impact of Covid19, have proved to be important: air quality difference (Eastern France, the Po Valley in Italy, Silesia in Poland…) etc..
The present study should, hence, be considered rather as a draft, ideally to be continued by trained statisticians. Its goal is not career-related, aiming only at creating the starting point of a rational debate about the fear epidemy propagated under the “Covid19” debate.
DATA SHEET
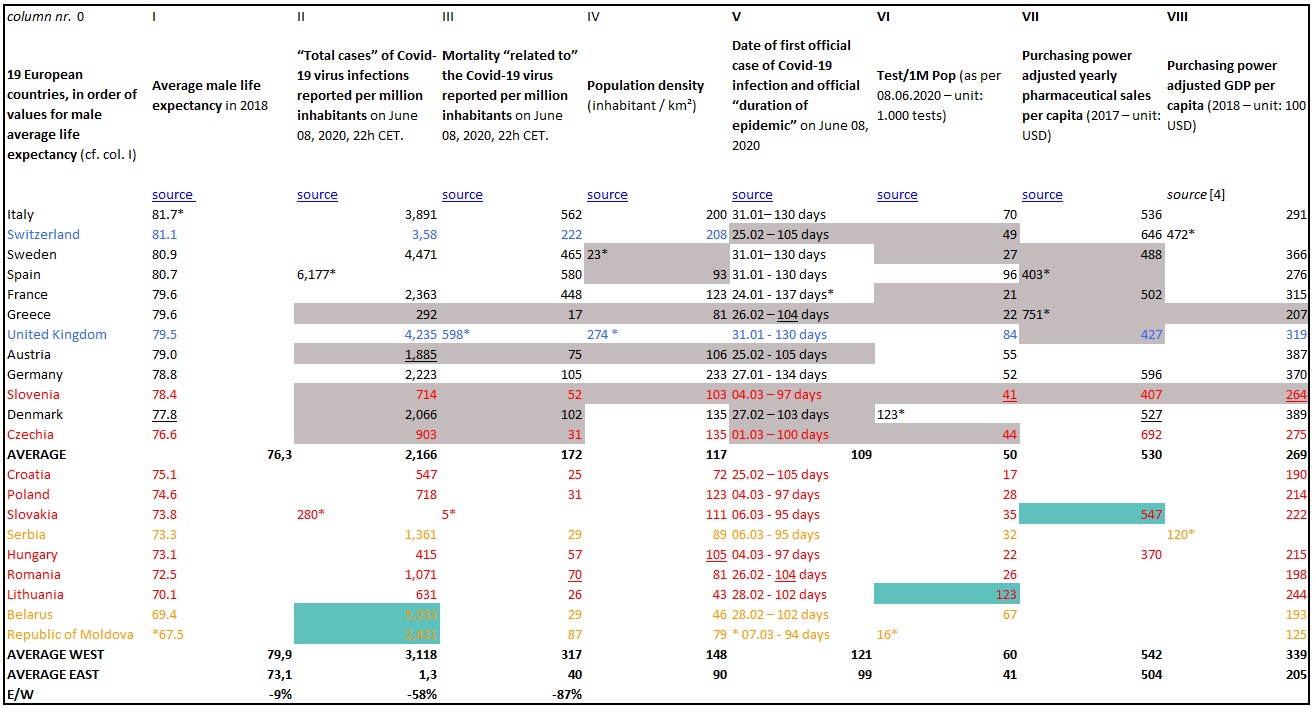
red: EU post-communist countries
yellow: post-communist countries not integrated into the EU
blue: non-EU Western countries
grey cell: values under the average of a column
turquoise cell: values above the average of a column
underlined: median values
* indicate countries with extreme values in a given column
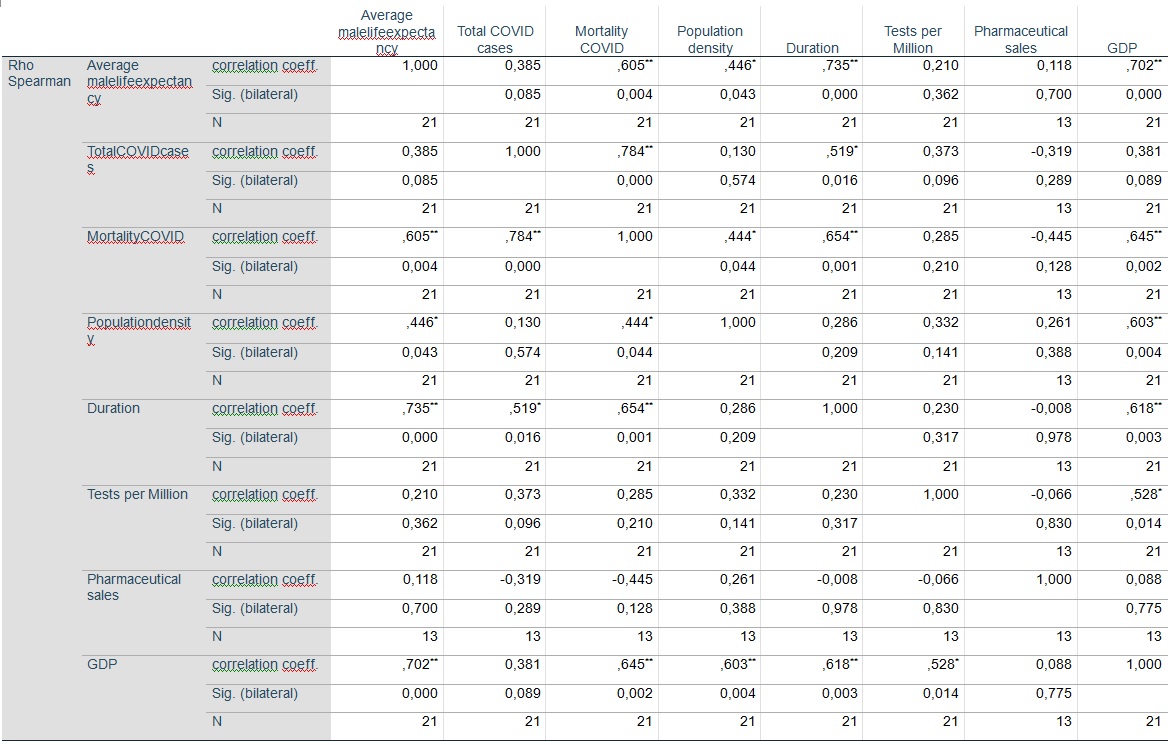
CORRELATIONS

INTERPRETATION
1. Incidence of population density:
This correlation is weak, even if, locally, the case of Greece, Austria and Slovenia could suggest some causal effect of population density. Density probably plays a role (as suggested, in addition to the studied group, by the case of the mega-states such as Russia and the USA), but the case of Sweden (the least densely populated state in the group, with a mortality level still typical for the Western category, though inferior to the one registered in most comparable quarantine states) suggest that such a causality is unlikely to be a predominant one.
Would the correlation be stronger, there would still be – as in the case of official duration – a doubt relating to the actual direction of the causal vector, as we can probably suspect a more general causality related to poverty: with a negative balance of migration, poor countries are both less populated, and plagued with lower life expectancy, hence have lower values in column III.
In other words: the results in col. IV, as well as those in col. III (via col. I) might both be consequences of those reflected in col. VIII.
2. Incidence of official duration:
As can be seen, the duration/mortality correlation is relatively strong. But it is worth noticing that the longevity/duration correlation is also strong. What does this mean?
In the data table, we present the date of the first “cases” in each country, specifying that they are “official” dates. In fact, if we take into account the recent high level of interconnection between Western Europe and the Eastern EU (and Eastern Partnership) countries, the official 22 day gap between the average duration of the two subsets seems unlikely, and evidence of previous infections is accumulating (although scarcity of tests, especially before the official “beginning”, as well as the ill-will of governments, make it difficult to clarify the issue).
In fact, I believe that the “link” between regional mortality rates and the official chronology of the epidemic is probably the opposite of that mentioned in most official speeches: in an area where Covid-19 had little lethal impact, one could actually expect the official alert to be given later – in fact rather under media pressure, with Eastern Europeans being culturally (and not only) dependent on Western models. Without the hysteria created in the West, it is very likely that the Covid-19 virus would have gone unnoticed in Eastern Europe – where its demographic impact, up to now, remains statistically invisible – as it will probably remain invisible in some Western countries (because, on an annual basis, the dying would … die anyway, with or without Covid-19). The death tolls of quarantines, on the other hand, is likely to become visible soon.
In other words: the direction of a possible causal link seems uncertain: it is very possible that older populations, therefore more vulnerable – especially where a higher percentage of that population lives in nursing homes –, will produce earlier warning signals than the least demographically vulnerable. Formulated differently: the values in col. III and V might in fact be both causally influenced by those in col. I (which, in turn, is largely influenced by the values in col. VIII).
The only scenario in which duration might have a real impact is the scenario of early (hence efficient) border-locks. Indeed, official duration, even if it would turn out that it reflects rather poorly real duration, certainly determines to some extent the precocity of border-locks (in countries which have implemented border-locks).
Greece, for instance, shows an odd combination of high male longevity (equal to the French value) and low mortality-rate (only Slovakia shows a better rate – but Slovak males live in average 5.8 year less than their Greek counterparts). As confirmed by the similar figures of neighbouring Cyprus and Malta, insularity may also have played a role, by reinforcing the efficiency of border-locks. Indeed, closing down an island is more akin to the initial (maritime) concept of quarantine than the so-called quarantine (better called: confinement) of the pseudo-scientific Fergusonian-Chinese model, which is really a quarantine per say: in France, Romania etc., people (including elderly) were still allowed (though under harsh and humiliating conditions) to go out of their homes from time to time to buy (at least) food, i.e. to engage in highly infectious contact with highly exposed people (retailers). “Closing down” a society, as a nearly impossible objective under the conditions of modern life, does not equal to closing down a country – even if politicians and media demagogy have tended to oversee this difference. The rather bad results of France (which had a fierce internal lock-down but permanently refused – for ideological reasons – to close down its borders) might be partly explained by not understanding this crucial difference (or not acting accordingly to such an understanding).
This, however, does not automatically “rehabilitate” duration as a key-factor: Denmark, with almost the same duration as Greece (and a slightly lower life expectancy), shows more than 5 times worse results, in spite of also being partly insular. On this topic as on others, obviously, more research is needed. Such a research, however, is impossible at the present stage, and might remain difficult in the years to come, as long as no massive and randomized immunity testing will be conducted, especially in countries where the Covid-19 virus is supposed to have had a late arrival (i.e., in our study, before all Eastern European countries). Considering the political effect which high immunization figures might have in such countries where a probably useless and economically devastating quarantine has been forced upon the population, one might fear, however, that such testing will never be conducted – or, if it is, that its results will not be published in an undistorted way.
3. Incidence of “Total cases”:
The correlation between this indicator and mortality is strong, but most likely due to an observation bias.
Since, in most European countries, testing has been done mostly (if not exclusively) on treated patients (+ their acquaintances, via contact research), i.e. on symptomatic patients with relatively severe symptoms, this kind of testing is likely to reflect more the potential of lethal impact on a given population than the actual prevalence of the infection in the same population. In other words: col. II is likely to be the shadow of col. III.
This is why, from a very early stage of this research, I chose to consider population-related mortality as the only reliable indicator of the epidemic impact, for one simple reason: there are asymptomatic patients, but there are no asymptomatic deaths. Therefore, the so-called infection figures (which should actually be called: positive testing figures) are dependent on the scale and effectiveness of testing policies, which in general in Europe (at first mainly due to lack of technical means – later on maybe also due to political ill will) have been very “modest”. There are, of course, unregistered death cases (e.g. deaths at home), but their very existence actually casts an additional shadow over the catastrophism used by health dictatorships – since anyone can see that, in this case, statistical uncertainty arises precisely from the fact that the dreaded Covid-19 … kills mostly the dying.
One of the statistical symptoms of “Total cases” being an unreliable indicator is its lack of correlation with longevity, while both the longevity/mortality and “Total cases”/mortality correlation is strong: in my opinion this is due to the fact that 1) after being tested positive, a patient has increased chances of dying with Covid-19, but 2) testing of asymptomatic people is neither randomized, nor methodologically homogeneous.
4. Incidence of longevity:
Of all potentially significant correlations, this is the strongest one.
This suggest that, immediately after obtaining population-corrected lethality data (i.e.: lethality/X inhabitants, instead of raw numbers), the first thing to do in order to have internationally comparable data is to submit the population-corrected data to a longevity-correction. Only longevity-corrected figures should allow for meaningful comparisons.
This is the purpose of the following section (section 7).
5. Incidence of medicine-consumption habits:
This takes us back to prof. Raoult’s April 14 interview, which provided for the initial impulse of the present study. Indeed, the aspect he emphasized most in that interview was not even demographics, but medicine-related habits.
This is, indeed, another common consequence of richness: inhabitants of rich countries generally have the means (either out of their own individual revenue, or thanks to mutualized healthcare systems) to become the target of Big Pharma’s pushing, i.e. to consume a lot a new drugs. Two things most new drugs (including vaccines) have in common, are:
- They are still under copyright, hence it makes sense for Big Pharma to advertise and push their use in the public (using or not its capture of expertise to achieve this goal).
- In spite of the commercialization permits they obtain (in many cases through captured expertise), they are generally not sufficiently tested.
In other words: rich citizens of the “Fist world” are typically not only the payers of “pharmaceutical progress”, but also its (generally unwilling) test-mice, while citizens of poor countries, gaining access to substances when they become generic, not only pay a lower price, but also take a lower risk.
One element of our study that might tend to confirm this hypothesis is the relatively bad results of Eastern European countries which have a significant part of their population living and working most of the year in some Western European country with a bad Covid-19 lethality-balance: Moldova and Romania (with around 25% of their population abroad, a big part of it in Italy, Spain and France). Those EU-internal migrants often have access to Western health structures and are culturally conditioned to consider any Western innovation as a very desirable thing (as opposed to their “retrograde” homeland’s culture).
This hypothesis, however, could only be confirmed by studying a more complete database of medicine-consumption habits, since
- the figures we have found do not cover all the countries of the study,
- the “pharmaceutical sales” figures are not as telling as would be more specific data on the consumption of new VS old medicinal substances, and
- even such data should of course ideally be corrected according to the general health condition of the populations (which is known to show ample variations, depending, among others, on eating, drinking and smoking habits).
Under such (provisory) conditions, the absence of any strong correlation with our “pharmaceutical sales” indicator is not surprising, and probably not very telling either.
6. Incidence of quarantines:
Since it is nearly impossible to quantify (in spite of some common traits) the very divergent quarantine policies of the 19 quarantining countries of the present study (and even more so the actual effectiveness of such measures, i.e. obedience levels within populations), I renounced including such policies in my correlation calculations.
People in favour of quarantine policies would argue that smaller lethal impacts should be explained, as often as possible, by the implementation of such policies. Unfortunately for them, I fail to see any proportionality between the existence or rigorousness of quarantines on the one hand, and national Covid-19 lethality figures on the other hand.
Even in the longevity-factor-corrected ranking (cf. infra), Sweden’s mortality is still lagging behind four rigorously quarantined countries – three of them (this is a remark for the fans of chronological causality) have acknowledged the presence of the virus on their territory on the very same day as Sweden. And Hungary, which is fiercely pro-quarantine in its internal political discourse, but actually implemented a kind of half-quarantine (with no real internal traffic restrictions, all shops open until 3PM, very few fines etc.) has better results than Romania, which instituted the fiercest quarantine of them all.
So this is, obviously, an illusion. Quarantine policies have never worked in the past – why should they have succeeded this time?[5]
As for the self-legitimizing “scholarship” of the London Imperial College, it hardly deserves any attention: according to them, quarantines saved the life of 3,1 million Europeans, i.e. of 0.42% of the European population. In accordance with such figures, Sweden, not implementing any mandatory quarantine, should have lost around 43 000 citizens. As we all know, the actual Swedish Covid-19 death toll represents hardly more than 10% of this figure.
7. Incidence of other factors:
“Popular science” flourishing during the Covid-crisis has come with a high number of explanatory hypothesis, mostly in order to explain the very striking East-West gap (see also: section 2 above). Let us mention one or two such explanations, which we have not deemed convincing enough to include them in our correlation-study.
- One of the basic assumptions of the present study is that people in Europe do not differ genetically enough to justify huge lethality differences when the (primary or secondary) death cause (in this case: a Covid-19 infection) is the same. Confronting blood-types or DNA-haplogroups maps with the geography of Covid-19 mortality immediately shows the absence of significant correlations. From the point of view of blood-types, the population of Greece has a lot in common with that of Italy and Spain (duration gap: 26 days). It is also well-known that on the average, Hungarians (10th/21 position in the longevity-corrected ranking below) are nearly indistinguishable from Croatians (19th/21 position) – the duration gap between both countries being only 8 days.
- The only treatment method known to have yielded good results (the one used by Prof. Raoult’s team in Marseille) has not been implemented nation-wide (let alone generalized in Europe). And the predicted jamming of health structures by the predicted “exponential peak” of infections actually happened in very few places, such as Northern Italy (where such jamming is actually a customary yearly event). Under such conditions, in spite of all the media- and politics-fuelled debate about health systems in various European countries, it seems unlikely that differences in health structures could provide a significant indicator.

LONGEVITY-CORRECTED DATA
There is, medically, an obvious connection between longevity and the lethal impact of virus (cf. supra). The reality of this connection, of course, can only be asserted in individual cases. Compared to individual diagnosis and biopsy, even age-pyramid-based statistics are generalizing and introducing fuzziness in the picture, let alone calculations based on national longevity averages. I consider, however, that, for the sake of nation-to-nation comparisons, there must be some proportionality between such longevity average-based calculation and the reality of individual cases.
The two non-quarantine countries of the present studies (Sweden and Belarus) having very close population numbers, but a longevity gap of 11.5 years, show a 94% mortality gap. We could, thus, posit that each of those 11.5 years “produces” an 8.17% mortality difference.
The same calculation, based on the data published by two fiercely quarantine countries, France and Romania (84% mortality gap for a 7.1 years longevity gap) would yield a 11.8%/year correction key.
An alternative calculation method[6] would be to “distribute” the 87% interregional mortality gap between the 6.8 years of difference between the two regional longevity-averages. The longevity correction key would then be 12.8%/year.
A similar distribution of our 60% longevity/mortality correlation (cf. section 5 supra) would yield a result closer to the Sweden/Belarus calculation.
Let us, for the sake of simplicity, adopt an 11% correction key (very close to the average of the aforementioned values).
This is, obviously, a very rough simplification of reality, since one can hardly believe that the impact of age on viral fragility could be scalar, i.e. that a 68-69 age difference would have the same impact as a 78-79 one. Of course, the correction key could never be used to predict individual outcomes, but it might help bettering the comparability of national data.
This general correction factor should of course generate individual (country-specific) correction-factors, by multiplying this 11% key by the (positive or negative) difference (in years) between a given country’s male life expectancy and the general average (which, in this study, is of 76.3 years).
E.g. for Germany:
(76.3 – 78.8) x 11 = -2.5 x 11 = -27,5% (rounded: -27%)
Hence Germany’s longevity-corrected relative lethality will be: 105 -27% = 76.65 (rounded: 77)
For Poland, on the other hand:
(76.3 – 74.6) x 11 = 1.7 x 11 = +18,7% (rounded: +19%)
Hence Poland’s longevity-corrected relative lethality will be: 31 +19% = 36.89 (rounded: 37)
After application of this correction factor, our data table looks like this:
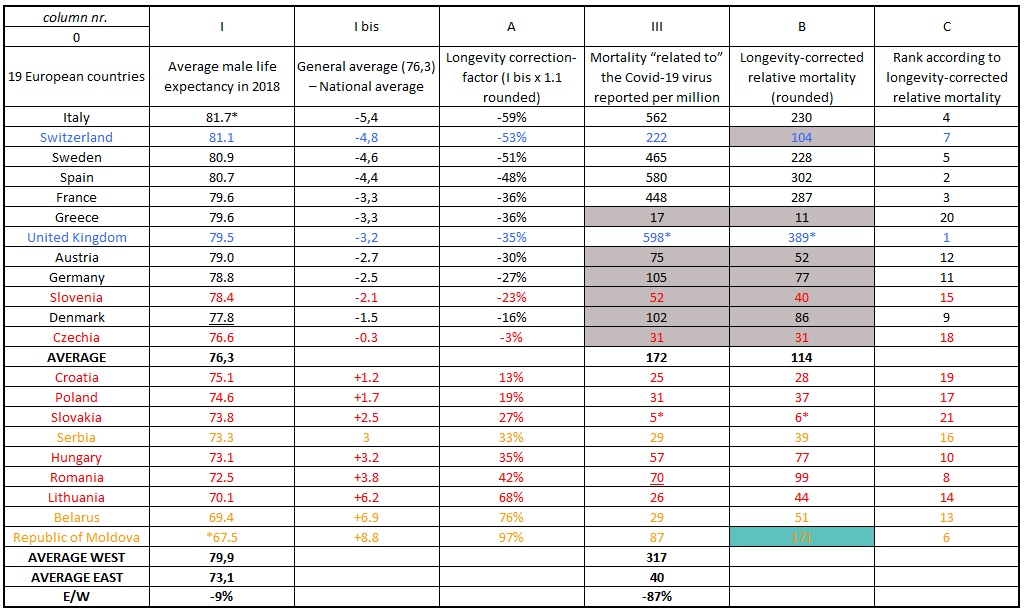
If we reorder the countries according to longevity-corrected mortality figures on June 8, we get:
United Kingdom > Spain > France > Italy > Sweden > Republic of Moldova > Switzerland > Romania > Denmark > Hungary > Germany > Austria > Belarus > Lithuania > Slovenia > Serbia > Poland > Czechia > Croatia > Greece > Slovakia
As can be seen, in spite of some level of correction (affecting positively the German-speaking world, and negatively the Romanian-speaking world), the top-10 of most affected countries still includes 7 Western countries, while the top-10 of least affected countries only includes 2 Western countries, with one more Western country (Germany) left in the middle.
So it would probably be as wrong to assert that Belarus’ figures are proving wrong French policies as to use Hungary’s against the “Swedish model”.
Both Western “winners”, however, as well as all the three Eastern “losers” of the longevity-corrected ranking were quarantine-countries. Non-quarantine countries do not show extreme values within their group, nor in the general classification.
In other terms: while providing a somewhat cleaned picture of the Covid-19 mortality, longevity-corrected figures do not “prove wrong” the quarantine policies, but certainly do not advocate in favour of such policies either.

GENERAL CONCLUSION
By comparing the demographic structure of the specific lethality of Covid-19 to the demographic structure of the population of post-communist countries (with an average male life expectancy under 74 years), as soon as the end of the first month of the “crisis” (the latest), one could deduce the improbability of scenarios predicting “exponential peak” (of potentially lethal diseases), supposed to lead to an overload of health systems. Let’s not forget that this is the very prediction which was supposed to justify the emptying of hospitals (which probably provided the bunk of quarantine-related victims as far).
Therefore, the measures adopted on the basis of such scenarios were epidemiologically unjustified.
The consequences of this failure of state expertise most likely produced a worse health record than that locally associated with the pandemic itself.
Causes of failure:
- In the West, where the above aberrant scenarios were born, they are probably related to the neoliberal devastation of medical intelligence and the capture of expertise by the pharmaceutical industry, thus the disappearance or adulteration of the very concept of public health.
- In Eastern Europe, servile imitation of this flawed Western model (as of many others) can be explained by the lack of a collective self-perception as a group of peoples economically, but also demographically, culturally, etc. distinct from the West, and the automatic, unreflective adoption of Western slogans in any field.
—
[1] The first published draft of the present study examined only 19 countries, with epidemic data from May 15. This second draft is based on epidemic data from June 8, also adding Greece and Belarus to the list of countries under scrutiny.
[2] Unless we compare longevity-corrected figures – cf. infra.
[3]Cf. ZELMAT, M, “Facing COVID-19 by the Confinement : EBM, ‘MBM’ or ‘SBM’?” (May 13, 2020). Available at SSRN: https://ssrn.com/abstract=3600511 or http://dx.doi.org/10.2139/ssrn.3600511
[4]Moldova and Belarus data from : https://data.worldbank.org/indicator/NY.GDP.PCAP.PP.CD?end=2018&locations=MD&start=2018&view=bar
[5]Cf. ZELMAT, op. cit.
[6] Used in an earlier published draft of the present study.
—
This article has been originally published in French on May 19, 2020. The original translation was a simplified, shortened version of the original article in French and has been provided by the author. On June 14, the author provided a second draft, which is the present article and replaces the former one, and which includes several new elements and considerations.
The points of views expressed within this article are those of the author and do not necessarily reflect those of the editors.