| IN A NUTSHELL |
|
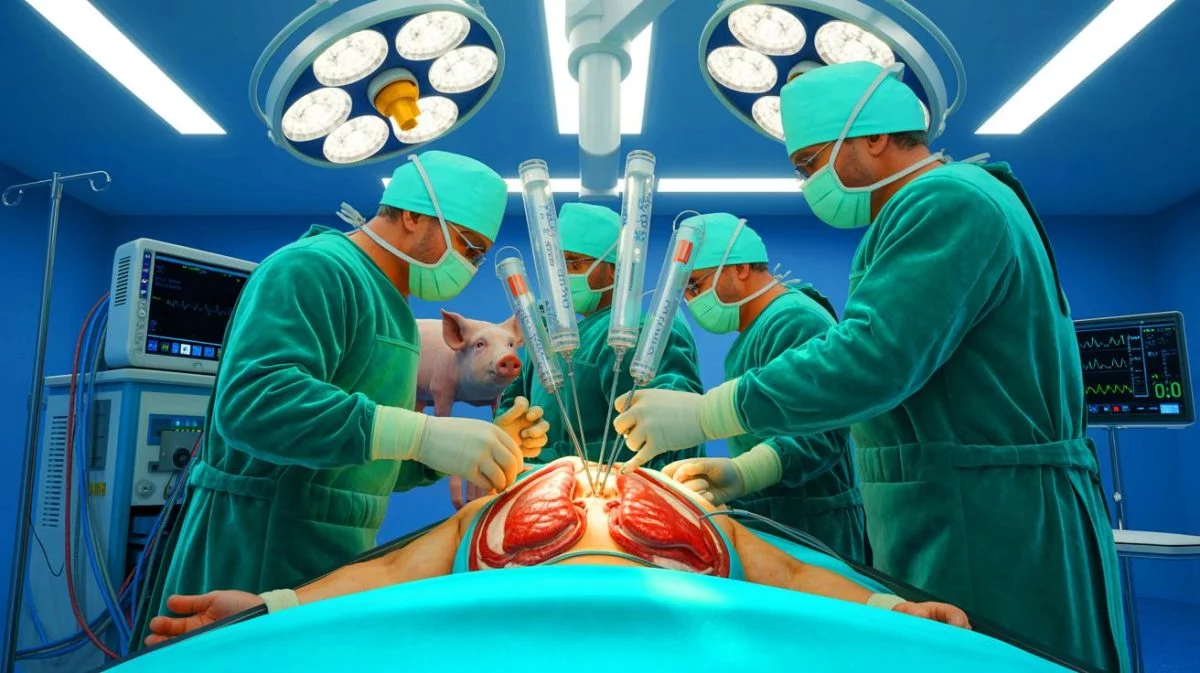
In an unprecedented medical milestone, a genetically modified pig lung was transplanted into a brain-dead human, marking a significant step in the field of xenotransplantation. This groundbreaking procedure was conducted by surgeons at Guangzhou Medical University in China, utilizing a lung from a Chinese Bama Xiang pig. The transplant managed to function for nine days, providing crucial insights into the viability and challenges of cross-species organ transplants. While the pig lung was able to oxygenate blood and expel carbon dioxide effectively, the experiment highlighted the complexities of organ rejection. The results offer a glimpse into the future potential of addressing the global organ shortage crisis.
Understanding The Organ Rejection Challenge
Xenotransplantation, or the transplantation of animal organs into humans, represents a promising frontier in medical science. As the World Health Organization reports, the current organ supply meets only about 10% of global transplant demand. In the United States alone, over 103,000 individuals are on waiting lists, with demand far exceeding the number of available organs. The ability to use genetically modified animal organs could significantly alleviate this crisis.
Among the organs, lungs present a particularly formidable challenge due to their highly reactive immune systems. The pig lung transplant, despite initial success, encountered complications. Within 24 hours, the lung began showing signs of damage and fluid accumulation. By days three and six, a progressive immune attack led to antibody-mediated rejection, culminating in the termination of the experiment on the ninth day. Professor Peter Friend from the University of Oxford noted that the recipient’s brain-dead state might have exacerbated these issues, as brain death can trigger inflammatory responses.
The Role of Genetic Modifications
The pig used in the transplantation belonged to the Bama Xiang breed, sourced from ClonOrgan, a biotech company in Chengdu, China. This miniature pig had undergone precise genetic modifications using the CRISPR genome editor. Specifically, three genes were knocked out to prevent immediate immune rejection, while three human genes were introduced to curb dangerous blood clotting.
Experts outside the study have emphasized that the use of pig lungs in human patients remains a distant goal. The research team itself acknowledged the need for further refinement, stating,
“Although this study demonstrates the feasibility of pig-to-human lung xenotransplantation, substantial challenges relating to organ rejection and infection remain, and further preclinical studies are necessary before clinical translation of this procedure.”
While this development is a notable advance, it is only a small step toward a long-term solution to the organ shortage.
Beyond Xenotransplantation: Exploring Alternatives
While xenotransplantation holds promise, it is not the only solution being explored to address organ shortages. Research is underway in other innovative areas, such as using stem cells to remodel donor organs and growing humanized organs within animals like pigs and sheep. These approaches aim to create organs that are more compatible with human bodies, potentially reducing rejection risks and increasing transplant success rates. The recent study, published in the journal Nature Medicine, highlights the complex interplay of science, ethics, and medicine in this evolving field.
As researchers continue to push the boundaries of what’s possible, the hope remains that a combination of these techniques could one day resolve the organ shortage crisis. The journey is fraught with challenges, but each step forward represents a significant contribution to medical science.
Implications and Future Directions
The successful integration of a pig lung into a human, even temporarily, opens new avenues for scientific inquiry and medical innovation. It raises questions about the ethical implications of cross-species organ transplantation and the potential risks involved. As scientists work to overcome the hurdles of rejection and infection, the ultimate goal is to create a seamless transition from animal to human organ use.
This landmark experiment prompts us to consider: what are the next steps in the quest for viable, long-term solutions to the organ shortage crisis? Could we see a future where genetically modified animal organs become commonplace in human medicine? The answers to these questions will shape the future of transplantation and the lives of countless individuals awaiting lifesaving procedures.
Did you like it? 4.5/5 (26)